[Norsk]
The United Nations Special Rapporteur on the right to health Mr. Pūras has called for «World needs “revolution” in mental health care». “There is now unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist”
To
Maria
Fagerbakke Strømme, Liv Solrunn Mellesdala, Christoffer
Bartz-Johannesenac, Rune Andreas Kroken, Marianne Krogenes, Lars
Mehlumd, Erik Johnsen. Copy: Working
group to update guidelines,
Robert Whitaker, Jari Tiihonen
Corrections and clarifications are suggested in view of how guidelines quote such studies. Correct guidelines will make patient’s informed consent valid.
Areas of concern are taken up. The wording of corrections and clarifications follow. The scientific basis and background is documented and recovery based treatment suggested by WHO guidance and the Council of Europe.
Conclusion: This study shows that discontinuation of antipsychotic drugs is associated with (but not causal for) more than twofold increased mortality risk in patients with schizophrenia. This problem can be reduced by reducing the number of FEP and acute patients medicated avoiding discontinuation problems.
Contents
Areas of concern
Corrections and clarifications
Scientific Basis
Recovery orientation
misrepresentation of retrospective covariant results as causal encourages guidelines to uphold this mistake
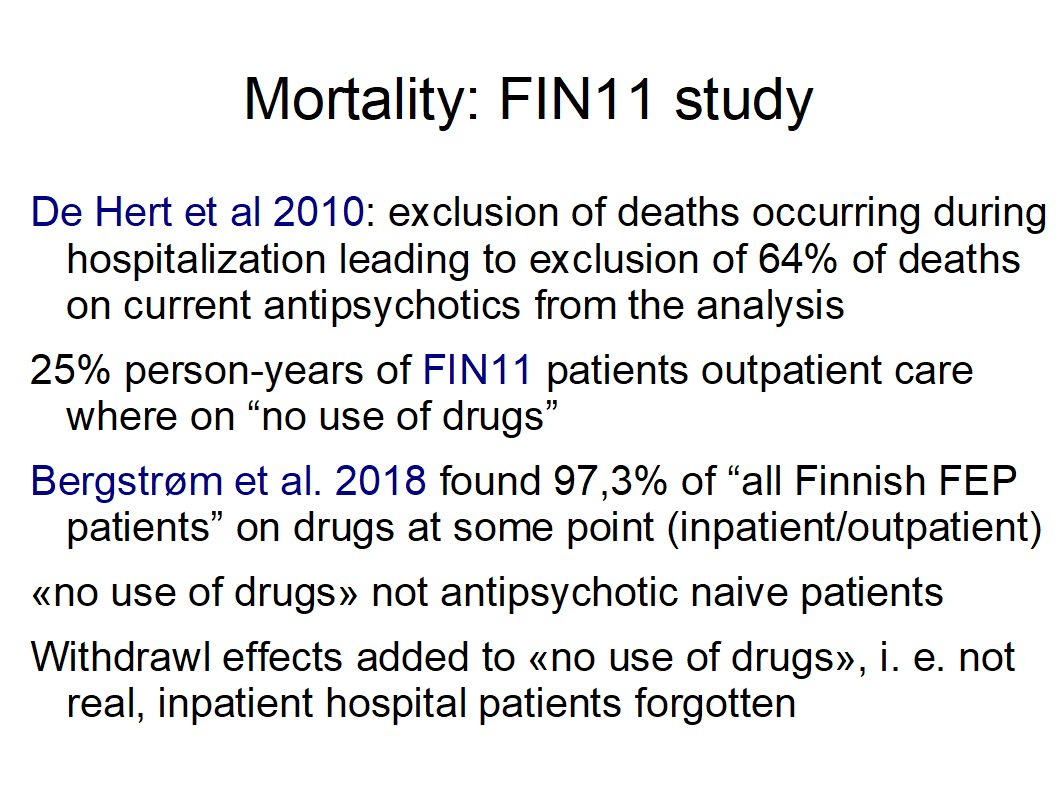
the study does not give the information how many of the patients are prescribed antipsychotics during acute admission and how many have been subject to forced drugging. 97,3% receive antipsychotics according to Bergstrøm et al 2018 at some point
“non-use of antipsychotic drugs” should be replaced by “discontinuation of drugs” to help guideline writers and readers understand that the study is not about FEP use and avoid the wrong conclusion that antipsychotics for FEP and acute use of drugs reduces mortality
evidence for prescribing antipsychotics is weak i. e. shows “It is uncertain if antipsychotics compared to placebo affects symptoms in persons with early psychosis because we have very little confidence in this result.” (FHI Dalsbø et al., 2019 )
there is not sufficient evidence for forced drugging
low unsure effect and side effects cause patients to cease medication
Cognitive behavioural therapy (CBT) has the same evidence in Norwegian guidelines as antipsychotics (1a, A). CBT should be offered to all. New studies e.g. Francey et al. 2020 and Morrison et al. 2020 strengthen this evidence
excessive use of psychotropic medicines is defended and even promoted
setting the methodological problems of the study aside, the conclusion is that prescribing antipsychotics in acute treatment should be much more cautious
however reducing excessive use of psychotropic medicines i. e. prescribing antipsychotics to fewer FEP patients can solve this problem
Council of Europe and WHOs promote voluntary and recovery oriented treatment show model programs with promising results
|
Text in study |
Suggested update |
|
Our results are in line with the study by Torniainen et al. (Torniainen et al., 2015) as well as a large number of studies concluding that use of antipsychotic drugs decreases the mortality risk (... Tiihinen et al., 2009 ...) |
Our results are in line with the study by Torniainen et al. (Torniainen et al., 2015) as well as a large number of studies concluding that use of antipsychotic drugs is associated with (but not causal for) lower mortality risk (... Tiihinen et al., 2009 ...) compared with discontinuation. |
|
Large register studies have demonstrated an increased mortality risk associated with non-use of antipsychotic drugs |
Large register studies have demonstrated an increased mortality risk associated with but not causal for discontinuation of antipsychotic drugs |
|
Antipsychotic drugs remain a cornerstone in treatment guidelines worldwide (Hasan et al., 2013; Lally and MacCabe, 2015). |
According to tradition, antipsychotic drugs have been a cornerstone in treatment guidelines worldwide (Hasan et al., 2013; Lally and MacCabe, 2015). However, FHI Jardim et al., 2021 finds: “It is uncertain if antipsychotics compared to placebo affects symptoms in persons with early psychosis because we have very little confidence in this result.” The use of psychotropic medicines is excessive (1) in spite of weak evidence. |
|
non-adherence rates as high as 40–75% (Lacro et al., 2002; Leucht and Heres, 2006). |
non-adherence rates as high as 40–75% (Lacro et al., 2002; Leucht and Heres, 2006) is due to low effect i. e. «god response» for acute reduction of symptoms for 9%, (Leucht et al. 2017 (“Sixty Years of Placebo-Controlled Antipsychotic Drug Trials”) and side effects i.e.. 94% (source) experience side effects. |
|
This study provides evidence that non-use of antipsychotic drugs is associated with more than twofold increased mortality risk in patients with schizophrenia. |
This study shows that discontinuation of antipsychotic drugs is associated with but not causal more than twofold increased mortality risk in patients with schizophrenia. However, withdrawal effects e. g. suicide risk weaken the results. These problems can be reduced by fewer patients receiving antipsychotics in acute settings. |
|
Although some studies on psychosocial interventions for schizophrenia without the use of antipsychotic drugs have been conducted, the evidence is generally of low quality (Cooper et al., 2020). |
Cognitive behavioural therapy (CBT) has the same evidence in Norwegian guidelines as antipsychotics (1a, A). CBT should be offered to all. It has been assumed that evidence for CBT is only obtained if antipsychotics are prescribed. However Cooper et al., 2020 has shown effects of CBT without the use of antipsychotic drugs. New studies confirm evidence «The selected sample recruited to this study, psychosocial treatment alone was not inferior to psychosocial treatment plus antipsychotic medication». (Francey et al. 2020). Morrison et al. 2020 concludes that CBT studies are save. |
|
it is evident that common adverse effects of antipsychotic drugs such as obesity, dyslipidaemia, and diabetes contribute to the increased mortality risk (Mackin et al., 2007). |
it is evident that common adverse effects of antipsychotic drugs such as obesity, dyslipidaemia, and diabetes contribute to the increased mortality risk (Mackin et al., 2007). Discontiuation of antipsychotic treatment will not remove this negative influence. This weakens the results of this study. |
The Norwegian guideline is wrong to assume causal relation. Causality cannot be claimed for sure in observational studies. Guidelines also claim that non-use of antipsychotics for FEP will reduce mortality. This cannot be concluded from register studies with all patients prescribed antipsychotics. Clarifications are necessary to guide those writing guidelines better in order to make patients’ informed consent valid.
Recent studies of the Norwegian Institute of Public Health (FHI) ISBN Jardim et al., 2021 found “It is uncertain if antipsychotics compared to placebo affects symptoms in persons with early psychosis because we have very little confidence in this result” because of lack of antipsychoticnaive studies. (Bola et al. 2011). “The use of antipsychotics cannot be justified based on the evidence we currently have. Withdrawal effects in the placebo groups make existing placebo-controlled trials unreliable.”
The United Nations Special Rapporteur on the right to health Mr. Pūras has called for «World needs “revolution” in mental health care». “There is now unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist”.
WHO followed up with: New WHO guidance seeks to put an end to human rights violations in mental health care:
“This comprehensive new guidance provides a strong argument for a much faster transition from mental health services that use coercion and focus almost exclusively on the use of medication to manage symptoms of mental health conditions, to a more holistic approach that takes into account the specific circumstances and wishes of the individual and offers a variety of approaches for treatment and support,” said Dr Michelle Funk of the Department of Mental Health and Substance Use, who led the development of the guidance.
Modell programs are e.g..: Open dialogue, Basal exposure therapy (BET), Heidenheim clinic and Soteria Berne.
Council of Europe suggests "Good practices in the Council of Europe to promote Voluntary Measures in Mental Health Services": «reduce, prevent or even eliminate coercive practices in mental health settings». Open dialogue, Basal exposure therapy and Safewards are role models.
WHO and Council of Europe guidance avoid forced drugging and overmedication of for many patients.
“The use of antipsychotics cannot be justified based on the evidence we currently have. Withdrawal effects in the placebo groups make existing placebo-controlled trials unreliable.” (Danborg et al. 2019).
American journalist covering medicine and science Robert Whitaker concludes in “Do Antipsychotics Protect Against Early Death? A Review of the Evidence.” «In both psychiatric and non-psychiatric patients, the use of antipsychotics doubles the risk of death in comparison to patients who do not take the medications.» The “antipsychotics lengthen lives” research of Jari Tiihonen is flawed in so many ways.
Bergström et al. 2018 compare FEP Open dialogue patients with all FEP patients in Finland over a period of 19 years. Open dialogue (OD) uses neuroleptics for 20% of patients in the beginning, standard treatment (CG control group) 70%. 97,3 % of the CG get neuroleptics at some point. At the end 36% of OD patients use neuroleptics, for CG it is 81%. Disability allowance, readmission and patients under treatment halves with OD (20). Standardized mortality ratio (SMR) decreases from 3.4 to 2.9 with OD. Mortality by illnes decreases from 9.2% to 2.8%. This register study describes facts / reality in Finland. Drastic reduction of neuroleptic use gives better treatment results
Assuming that Open dialogue area population is representative, this emulates randomisation-avoiding problems of selection because all patients are included.
Rindal, 1 September 2021
Walter Keim
Follow-up:
Posselt et al. 2021: The Danish OPUS Early Intervention Services for First-Episode Psychosis. “patients who received OPUS treatment after implementation (N=3,328) had a tendency toward lower mortality, fewer and shorter psychiatric admissions
Strømme et al. 2022: Use of Benzodiazepines and Antipsychotic Drugs “Use of medications Antipsychotics 93.2%”
Reference:
6 June 2017. The United Nations Special Rapporteur on the right to health: World needs “revolution” in mental health care – UN rights expert https://www.ohchr.org/en/press-releases/2017/06/world-needs-revolution-mental-health-care-un-rights-expert&LangID=E
May 2, 2020: Robert Whitaker: Do Antipsychotics Protect Against Early Death? A Review of the Evidence. https://www.madinamerica.com/2020/05/do-antipsychotics-protect-against-early-death-a-review-of-the-evidence/
Whitaker RB (2020). Rejoinder to commentary. Psychological Medicine 50, 2809–2809. https://doi.org/10.1017/S0033291720004109 https://www.cambridge.org/core/journals/psychological-medicine/article/rejoinder-to-commentary/66FA83EDE51B1731D8572336B52D965F
J Moncrieff · 2020: Misleading information about antipsychotics https://discovery.ucl.ac.uk/id/eprint/10124439/1/Moncrieff_PM_letter_301020.pdf